(https://peacebyjesuscom.blogspot.com/2019/10/negative-effects-of-homosexual.html). Last updated: 11-21-2025 by the grace of God.
Excerpt:
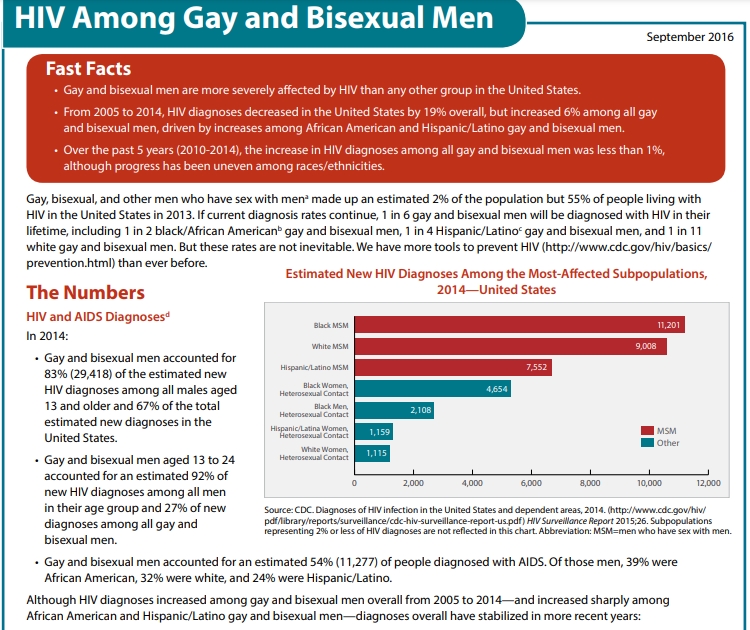
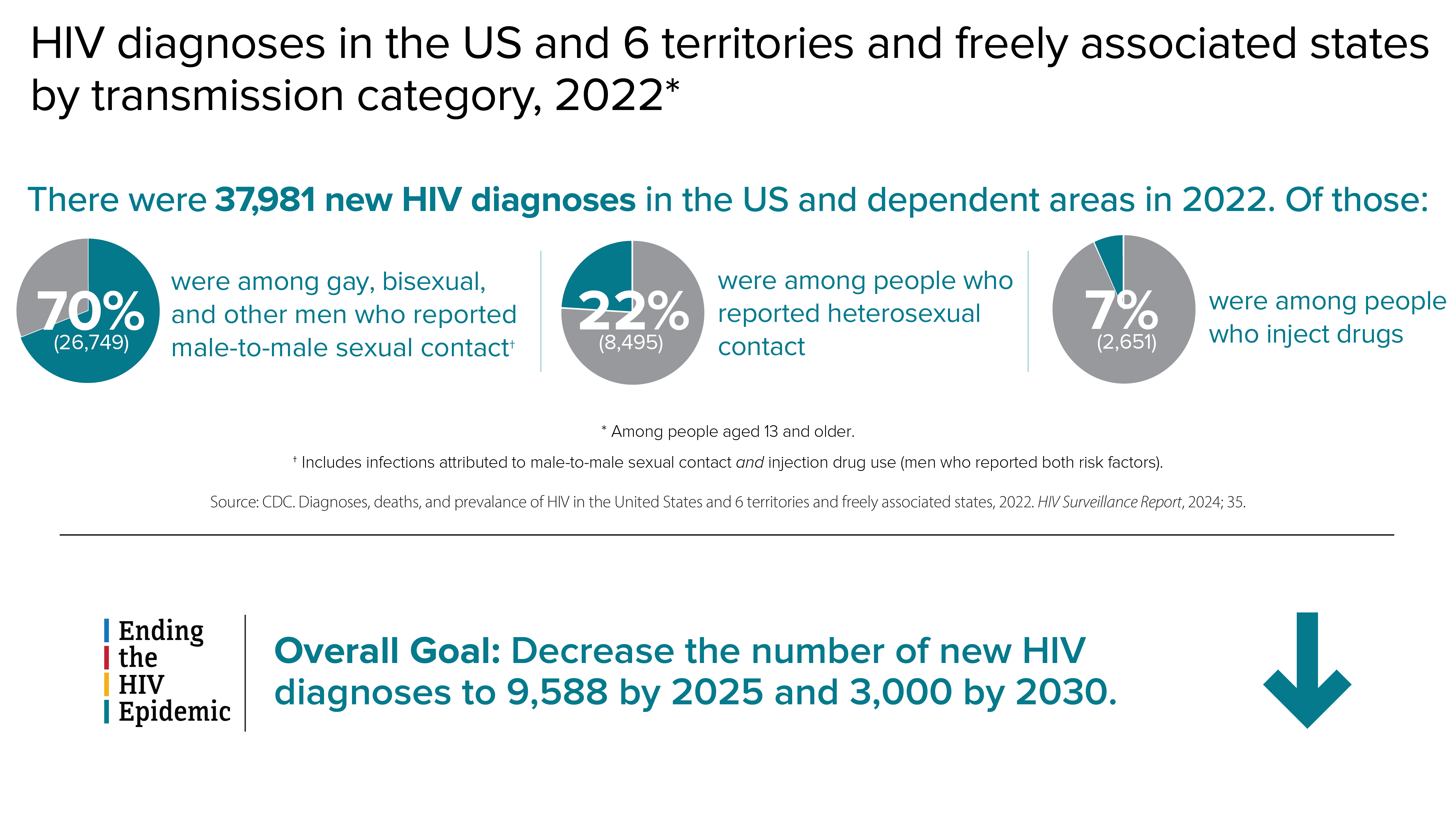
In 2021, gay, bisexual, and other men who reported male-to-male sexual contact accounted for 86% of estimated infections among all men (87% in 2022). Although only approximately 7% of adult and adolescent males reported having had male-to-male sexual contact at some point in their lives, over 80% of HIV infections among young males in 2019 were attributed to male-to-male sexual contact. and over over 63% of all [not just men] new HIV diagnoses. Overall, homosexual relations have (historically) resulted in a greatly increased incidence of other infectious diseases and effects besides HIV, from Meningitis to premature death. Which diseases includes Chlamydia, Gonorrhea, Hepatitis A and B, HPV, Syphilis, HIV to Meningitis and body dysmorphia and eating disorders and recently Monkey pox. Gay, bisexual, and other men who have sex with men have accounted for 83% of primary and secondary syphilis cases where sex of sex partner was known in the US. Goy, Bisexual and other men who have sex with men have been found to be 17 times more likely to get anal cancer than heterosexual men. In addition to which is accelerated aging and premature death, plus higher domestic abuse. Which practices costs this nation greatly in lives, souls - and money, with the latter alone meaning billions spent per year due to STD's, with overall Federal Funding for HIV/AIDS in FY 2022 alone being: $42.86 billion. And (as of 2025 extrapolation) sodomy has been primarily responsible for an estimated 750,000 American deaths due to HIV/AIDS. And yet all the above is not the decisive reason why homosexual relations are wrong (follow link). .
What follows is a progressively compiled piecemeal and thus somewhat disorganized (not all chronological, etc.) collection of statistics, mostly from between 2017 to 2021, with many images (almost all from the CDC) on sexually transmitted diseases/infections (STD's/STI's), mainly focusing on effects of homosexual relations and mostly between biological males). Yet which (unlike other search engines tested) Google ignores, consistent with liberal bias.
And yet, in anticipation of attacks on this study, let me say that this page is not presented as a self-righteous condemnation as if I (or any who cite this study) are without sin, for we are all sinners, having misused everything from our brain to our feet, and thus in this way and to some degree we and I have usually committed many or most things that we condemn others for, and our lesser sins that we may excuse are offensive to God and not just those that we may rightly deplore.
However, the difference here is that of having turned to the Lord Jesus from sin, and thus toward characteristic obedience to Him - including repentance from known sin - versus defending and even promoting sin.
And this page is particularly written in response to those who justify fornication, especially sodomy, and even promote it, and even attack dissent (which is one reason why it provokes more reaction). Many of such even attempt to argue against the Bible, but which teaches that God made man and women distinctively different yet uniquely compatible and complementary, and only joined them together in marriage - as the Lord Jesus Himself specified (Mt. 19:4–6) - and Scripture only unconditionally condemns homosexual relations wherever they aremanifestly dealt with (all sin is condemned, yet there are different degrees, and unlike some sins, there is no provision that will sanction homosexual relations).
And thus fornication is immoral/wrong even aside from the deleterious physical, mental and financial effects substantiated here.
However, most of all, may this compilation work to bring repentance and salvation thru effectual, penitent, regenerating justifying faith in the risen Lord Jesus, (Acts 10:34-47; 15:5-7; Titus 3:5) whom the Father sent to be the Savior of the world. (1 Jn 4:14) Thanks be to God, Amen
(https://web.archive.org/web/20250926221650/https://www.cdc.gov/hiv/media/images/2024/06/CDC-HIV-in-the-US_2024-09.png)
category, 2019—United States and 6 dependent areas
(https://web.archive.org/web/20211022161450if_/https://www.cdc.gov/hiv/images/group/gender/men/2020/cdc-hiv-men-diagnoses-bar-graph-700x318.png?_=96703)
While the CDC states that,
"Gay, bisexual, and other men who have sex with men (MSM) are the population most affected by HIV in the United States. Stigma, homophobia, and discrimination make MSM of all races/ethnicities susceptible to multiple physical and mental health problems,"
the means of HIV transmission is almost always due to volitional actions, which cannot be blamed on discrimination, while billions are spent on this communicable disease via a chosen practice.
Although only approximately 7% of adult and adolescent males reported having had male-to-male sexual contact at some point in their lives, 81% of HIV infections among [all classes of] males in 2019 were attributed to male-to-male sexual contact. (CDC: Estimated HIV Incidence and Prevalence in the United States, 2015–2019 P. 7)
Update: In 2023, 25,909 people were newly diagnosed with HIV attributed to male-to-male sexual contact, representing 66% of all new HIV diagnoses in the U.S. Among males, 81% of new diagnoses were attributed to male-to-male sexual contact. (https://aidsvu.org/resources/toolkits/gay-mens-hiv-aids-awareness-day-toolkit/)
And in 2018:
(from https://www.cdc.gov/hiv/pdf/group/age/youth/cdc-hiv-youth.pdf)
In 2020 the CDC reported that 92% of NEW HIV infections among men aged 13 to 24 was attributed to male-to-male sexual contact:
https://web.archive.org/web/20200407222113if_/https://www.cdc.gov/hiv/images/group/age/youth/cdc-hiv-youth-sex-700x698.png; https://web.archive.org/web/20210615095455im_/https://www.cdc.gov/hiv/images/group/age/youth/2021/04-68-medium.png https://web.archive.org/web/20190807143141im_/https://www.cdc.gov/hiv/images/group/age/youth/Piecharts-03-large.png)
https://web.archive.org/web/20190807143141im_/https://www.cdc.gov/hiv/images/group/age/youth/Piecharts-03-large.png)four percent of the male population in the United States, but
male-to-male sex accounted for more than three-fourths
(78 percent) of new HIV infections among men and nearly
two-thirds (63 percent) of all new infections in 2010 (29,800). (https://web.archive.org/web/20221215124259/https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf)
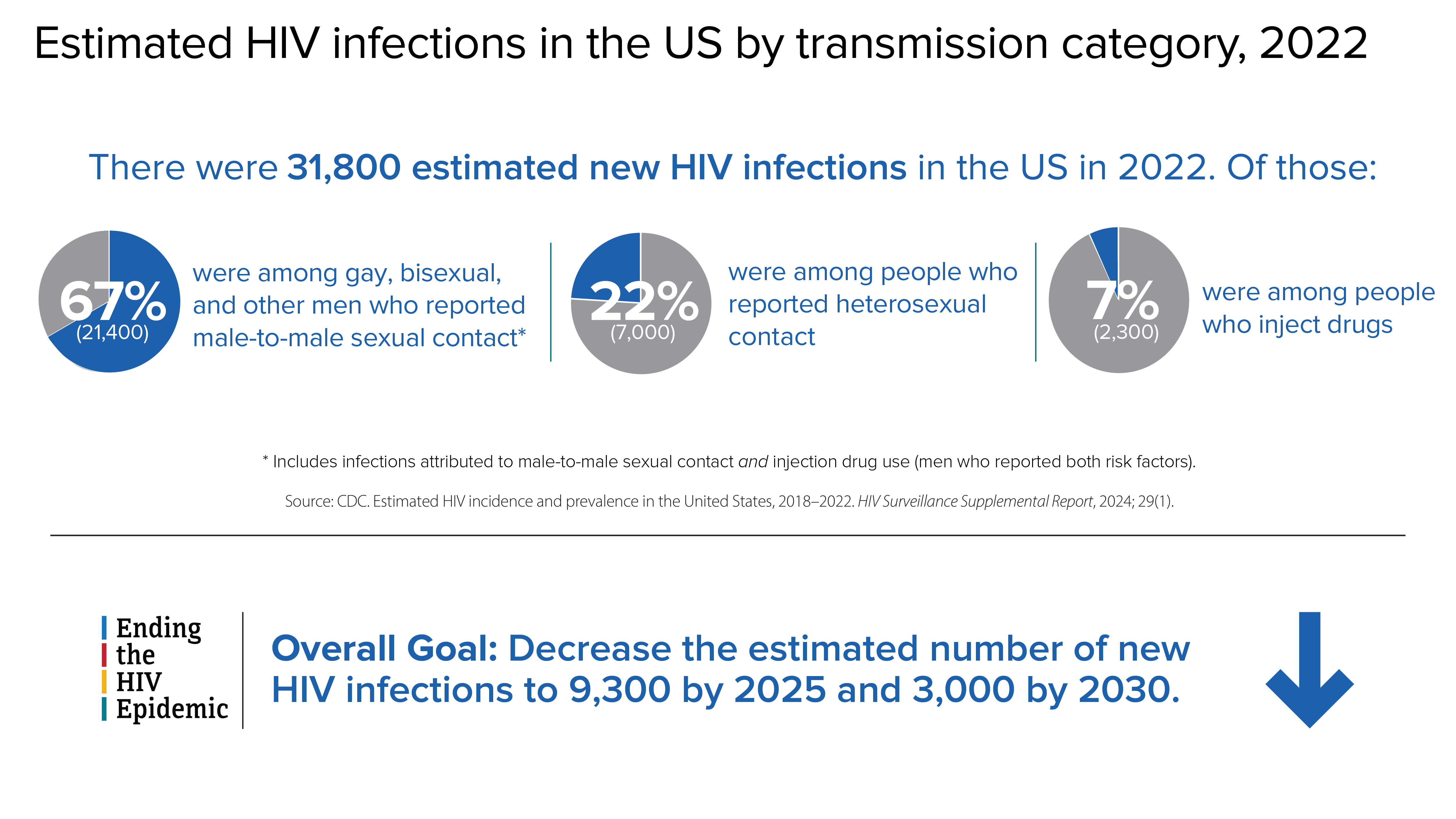
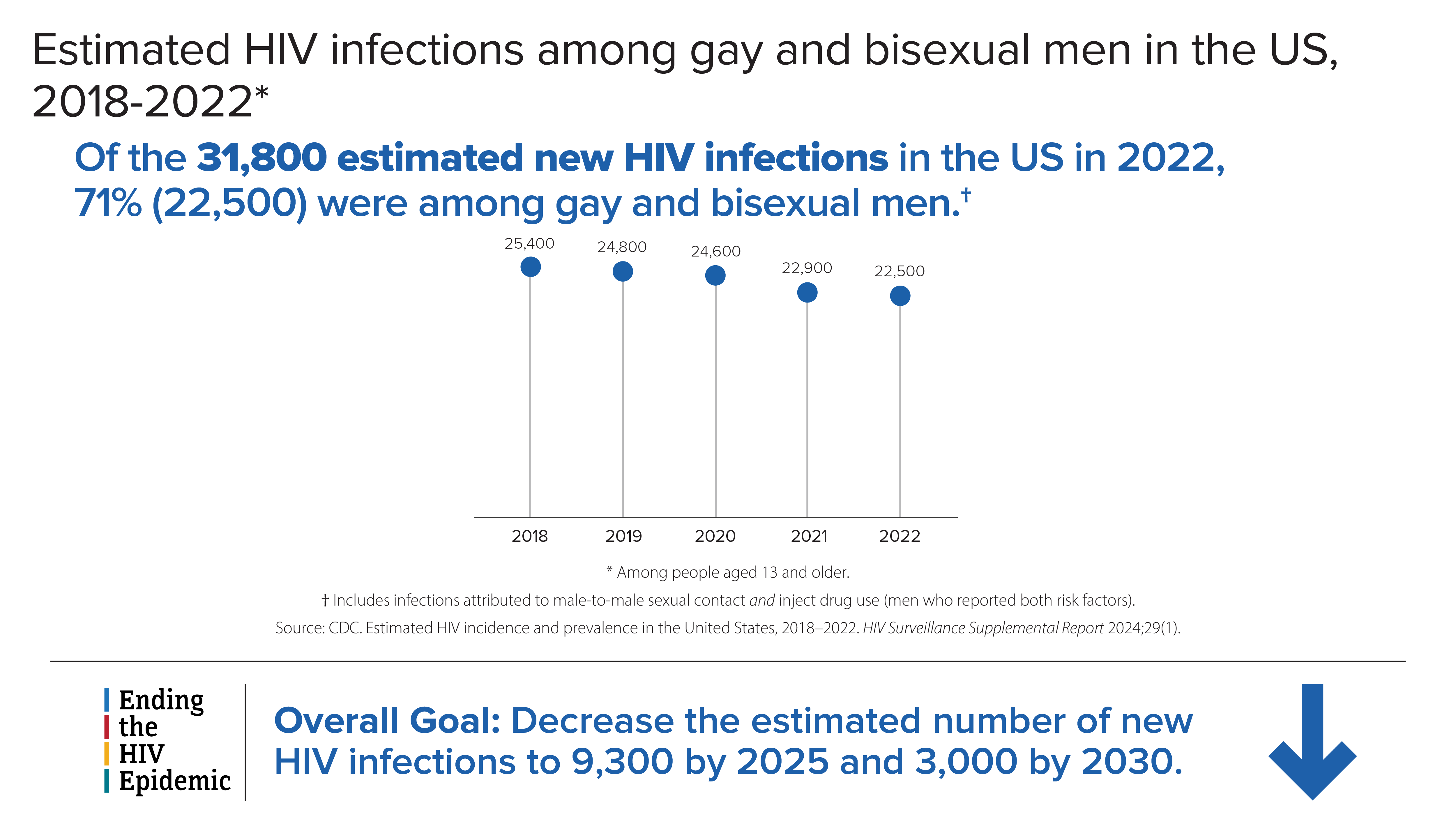
In 2019, gay, bisexual, and other men who reported male-to-male sexual contact accounted for 86% of estimated infections among all men. (https://www.cdc.gov/hiv/statistics/overview/in-us/incidence.html)
In 2019, the largest percentage of HIV infections among all was attributed to male-to-male sexual contact (66% overall and 81% among males). In 2019, among females, the largest percentage of HIV infection was attributed to heterosexual contact (83%).
For the receptive male the estimated average chance of contracting HIV can range from 1.38% - about one transmission occurring for every 71 exposures, male or female - (https://www.medicalnewstoday.com/articles/chances-of-getting-hiv) to over 20% - equivalent to 1 transmission per 5 exposures via unprotected sex with an HIV-positive person who has acute HIV infection.. (https://stanfordhealthcare.org/medical-conditions/sexual-and-reproductive-health/hiv-aids/causes/risk-of-exposure.html)
In 2016 the rate of people living with HIV per 100,000 population was 368, with the death rate being 6. Male-to-male
sexual contact made up 82.4% of HIV infections among males in 2017,
while heterosexual contact made up 85.7% of HIV infections among
females. The rate of Black males living with an HIV diagnosis is 5.6
times that of White males. The rate of Black females living with an HIV
diagnosis is 17.6 times that of White females. The rate of
Hispanic/Latino males living with an HIV diagnosis is 2.5 times that of
White males. The rate of Hispanic/Latina females living with an HIV
diagnosis is 4.2 times that of White females. (https://aidsvu.org/local-data/united-states)
The South has the highest number of people living with HIV, but if population size is taken into account, the Northeast has the highest rate of people living with HIV.
"Cumulative deaths in US through 2002 -- 501,669" due to or with HIV/AIDS. (https://www.factlv.org/timeline.htm)
"Since the beginning of the epidemic, nearly 675,000 people with AIDS in the United States have died, and even today, nearly 13,000 people with AIDS in the United States die each year." (https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf)
In 2020, there were 18,489 deaths among adults and adolescents with diagnosed HIV in the US and dependent areas. (https://www.cdc.gov/hiv/statistics/overview/index.html)
In 2021, there were 19,986 deaths among adults and adolescents with diagnosed HIV in the United States and 6 dependent areas. (https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics/)
"About 13% (153,500) of people with HIV in the U.S. don't know it and so need testing." (https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics/)
On Aug 16, 2024 KFFmedia reported that about 8,000 people die with HIV-related illness as a contributing cause of death each year. (https://www.kff.org/hiv-aids/the-hiv-aids-epidemic-in-the-united-states-the-basics/
Ignoring deaths among the undiagnosed, including the early years of the epidemic, and using rounded figures of deaths due to, or with HIV/AIDS per year,
However, the death rate was higher the further back one goes (yet by 2004 over 500,000 of deaths by or with AIDS being cited, (https://www.healthline.com/health/hiv-aids/facts-statistics-infographic#demographics) and with more recent data showing declines, with approximately 6,310 deaths being cited in 2021 . And yet the 700,000 figure of deaths due to AIDS has been cited since at least 2017 and onward without updating (a, b, c, d, e, f, g), and is still being quoted in 2025.
So in order to obtain a rough estimate, using higher earlier-year death counts, plus declining figures from recent years leads to a cumulative total deaths count of Americans that have died so far due to or with HIV/AIDS as being close to 750,000.
In 2019 in the United States and 6 dependent areas, diagnoses of HIV infection for adolescents and young adults attributed to MMSC (approximately 83%, including 3% MMSC and IDU) and those attributed to heterosexual contact (13%) accounted for approximately 97% of diagnoses in the United States.
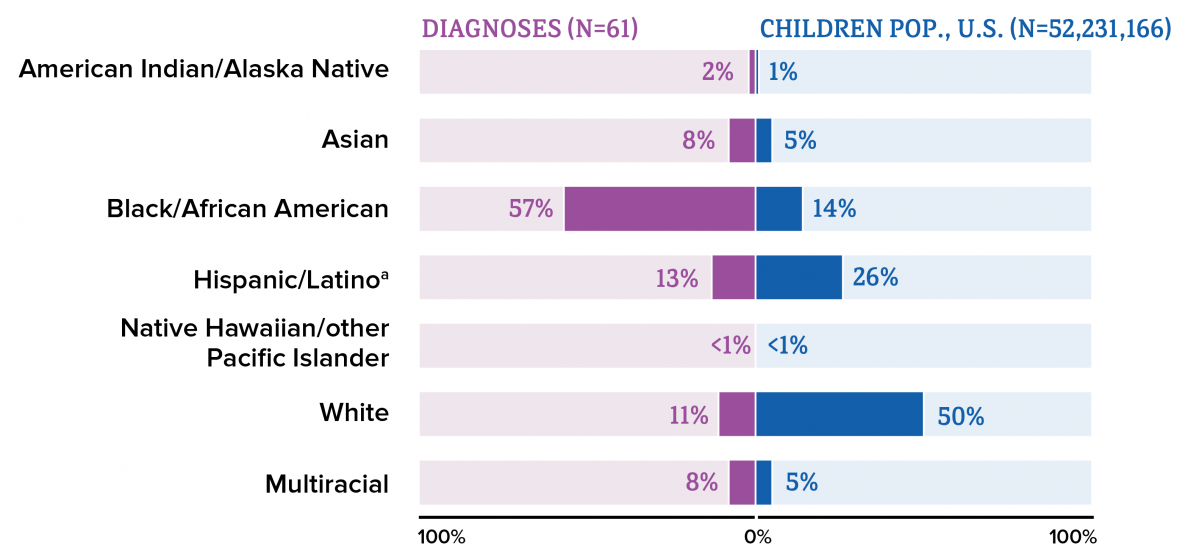
Asian female adults and adolescents had the largest percentage (93%) of diagnoses of HIV infection attributed to heterosexual contact, followed by Black/African American (91%), and Hispanic/Latino (87%) female adults and adolescents. In 2019, Black/African American children made up approximately 14% of the population of children but accounted for 57% of diagnoses of HIV infection among children. https://web.archive.org/web/20241130043141/https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2018-updated-vol-32.pdf
In 2019, among all Black/African American persons, males accounted for 76% of HIV infections, most of which (82%) were attributed to male-to-male sexual contact. (https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-26-1.pdf P. 6)In the 2015 UNAIDS (Joint United Nations Program on HIV/AIDS) report, studies in sub-Saharan Africa found prevalence rates of HIV infection ranging from 6 to 37%
among MSM
As the observed prevalence rate of HIV in the general population was between 0.1 and 19%, the prevalence rate among men who have sex with men (MSM) was often 13 to 17 times higher."
Gay, bisexual, and other men who have sex with men have accounted for 83% of primary and secondary syphilis cases where sex of sex partner was known in the US. Goy, Bisexual and other men who have sex with men have been found to be 17 times more likely to get anal cancer than heterosexual men. In addition to which is accelerated aging and premature death.
And yet all the above is not the decisive reason why homosexual relations are wrong.
Also, a new analysis (Oct. 11, 2024) reveals that infection with the mpox (money pox) virus is five times more likely among gay and bisexual men who engage in unprotected sodomy as the receptive partner, while clusters of mpox cases with are strain of mpox that is resistant to treatment have been reported. Of 1,500 American men under the age of 50 who said they had sex with other men 457 had contracted mpox. (https://www.usnews.com/news/health-news/articles/2024-10-11/unprotected-sex-boosts-mpox-danger-for-gay-men-as-drug-resistant-strain-spreads)
Related to this is that,
The risk of becoming infected with HIV during condomless anal sex is 10 to 20 times greater than condomless vaginal sex. Because the rectal lining is only one-cell thick, the virus can more easily reach immune cells to infect. (https://www.mtnstopshiv.org/news/rectal-microbicides-fact-sheet)
Also reported, "People living with HIV in Canada had eight times the risk of Alzheimer’s disease and other non-AIDS-related dementia as their HIV-negative counterparts, and they were diagnosed 12.5 years earlier [which in part may be due to more medical attention], according to an analysis published in BMJ Open.
They also had higher rates of several other age-related chronic conditions....Antiretroviral treatment has been associated with kidney damage and cardiovascular disease, and viral hepatitis and alcohol use—both common among HIV-positive people—can cause liver disease." (https://www.poz.com/article/people-hiv-diagnosed-dementia-13-years-earlier)
Gender non-contentedness, while being relatively common during early adolescence, in general decreases with age and appears to be associated with a poorer self-concept and mental health throughout development. - Rawee, P., Rosmalen, J. G. M., Kalverdijk, L., & Burke, S. M. (2024). Development of Gender Non-Contentedness During Adolescence and Early Adulthood. Archives of Sexual Behavior. Advance online publication. https://doi.org/10.1007/s10508-024-02817-5
A massive, yearslong study in Germany shows the overwhelming majority of young people who identify as transgender will grow out of the diagnosis within five years. Two out of three young people medically diagnosed with gender dysphoria will no longer identify as a member of the opposite sex within five years.The most likely group to change its mind is 15-to-19-year-old females, with 72.7% desisting. But a majority (50.3%) of young men who came to their transgender identity in adulthood (males aged 20-24) also desisted in five years. - https://www.dailysignal.com/2024/06/15/german-study-vast-majority-of-people-will-grow-out-of-transgenderism-within-5-years/
LGBTQ young people are more than twice as likely to feel suicidal, and over four times as likely to attempt suicide, compared to heterosexual youth (Kann 2016)
In a 2016-2017 survey from the Human Rights Campaign Foundation, 28 percent of LGBTQ youth — including 40 percent of transgender youth — said they felt depressed most or all of the time during the previous 30 days, compared to only 12 percent of non-LGBTQ youth (HRC Foundation 2017: https://suicidepreventionlifeline.org/wp-content/uploads/2017/07/LGBTQ_MentalHealth_OnePager.pdf)
A large study also found that of 10,270 transgender patients identified, approximately 58% of transgender patients had at least one DSM-5 diagnosis compared with 13.6% of cisgender patients, indicating transgenders had about 4.5 times higher rate of psychiatric illness than straight persons. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6830528/)
"41% of trans adults said they had attempted suicide, in one study. The same study found that 61% of trans people who were victims of physical assault had attempted suicide." (https://save.org/about-suicide/suicide-facts/)
In 2017 almost 35% of high school students who identified as transgender reported attempting suicide in the last 12 months (versus 9.% of straights), and almost 44% considered attempting it. Transgender students were much more likely to have ever had engaged in sexual relations than were cisgender (straight) females (43.1% versus 33.2%), and with more persons, while almost 15% reported their first act was before age 13 years vs. 1.5% for straights.
Also relevant, disputed (https://www.insidehighered.com/news/2023/03/20/journal-places-warning-flawed-abuse-homosexuality-study) research by Jessica Jones Steed and Donald I. Templer reported in 2010 that a study by Tomeo, Tem- pler, Anderson, and Kotler [1] found that,
56% of gay men in contrast to 7% of heterosexual men, and 22% of lesbian women in contrast to 1% of heterosexual women, had reported homosexual molestation. Previous research also reported a history of molestation in gay men and lesbians [2-6]. The Tomeo et al. [1] research went beyond the previous research in that they used specific criteria of molestation by requesting the gender and age of the perpetrator and by the determination of both current sexual preference and that before the molestation. They found that 32% of gay men and 38% of the lesbians reported they were not homosexual before the homosexual molestation.
Steed and Templer went further, engaging in a study consisting of 280 non-clinical adults from gay, lesbian, and bisexual organizations in Central California, in which 49.6% of males reported being gay and 50.4% reported being bisexual.
Of both gay/bisexual men and lesbian/bisexual women, females reported 57.3% being lesbians and 42.7% being bisexual. It found that 42 (30.7%) of the 137 males, 59 (41.3%) of the 143 females, and 101 (36.1%) of the total number of participants reported experiencing childhood/adolescent molestation. A high rate of molestation of homosexual persons has also been reported by other authors [2-4, 11, 12]
Of the male participants who reported homosexual molestation, 80.0% of the perpetrators were said to be homosexual, 4% heterosexual, and 16% of unknown orientation. Of the female participants who reported homosexual molestation, 94.4% of the perpetrators were said to be homosexual, none heterosexual, and 5.6% of unknown orientation.
Seventeen (67.4%) of the participants who were homosexually molested, in contrast to 26 (45.6%) of those who were heterosexually molested, said the molestation had an impact on their sexual orientation. (https://openpsychologyjournal.com/contents/volumes/V3/TOPSYJ-3-36/TOPSYJ-3-36.pdf)
According to a different study in the November 2009 issue of the International Journal of Child Abuse & Neglect, about 20 percent of men who have sex with men are sexually abused as children, a rate similar to that found among heterosexual women. The difference is that 80 percent of gay and bisexual men, compared to 20 percent of heterosexual women, who are sexually abused report experiencing "severe" abuse, often involving violence. Both men and women who are abused as children tend to engage in what researchers define as "high-risk" behavior as adults, which includes unprotected sexual encounters. (https://today.oregonstate.edu/archives/2008/dec/high-rates-childhood-sexual-abuse-contributing-factor-spread-hiv)
In 2013, the CDC released the results of a 2010 study on victimization by sexual orientation, and admitted that “little is known about the national prevalence of intimate partner violence, sexual violence, and stalking among lesbian, gay, and bisexual women and men in the United States.” The report found that bisexual women had an overwhelming prevalence of violent partners in their lives: 75 percent had been with a violent partner, as opposed to 46 percent of lesbian women and 43 percent of straight women. For bisexual men, that number was 47 percent. For gay men, it was 40 percent, and 21 percent for straight men. - https://www.smithsonianmag.com/smart-news/if-youre-not-stragiht-youre-at-higher-risk-for-domestic-violence-180949988/
2015: According to the CDC’s National Intimate Partner and Sexual Violence Survey (NISVS), there is a higher prevalence of lifetime experiences of IPV among bisexual women than heterosexual women (Walters et al, 2013). Bisexual women are 1.8 times more likely to report ever having experienced IPV than heterosexual women (see Table I).
According to the NISVS, bisexual women are 2.6 times more likely to report ever having experienced intimate partner sexual violence compared to heterosexual women.
According to the NISVS, bisexual men seem more likely to report ever having experienced IPV than heterosexual men, and gay men seem less likely than heterosexual men to report ever having experienced IPV. - https://williamsinstitute.law.ucla.edu/publications/ipv-sex-abuse-lgbt-people/
- 61.1% of bisexual women, 26% of gay men, and 37.3% of bisexual men have reported an experience of rape, physical violence, and/or stalking within an intimate relationship.
- 63% of lesbian women, 76% of bisexual women, 60% of gay men, and 53% of bisexual men have reported experiencing psychological aggression by a partner at some point in their lives.
- According to the National Coalition Against Domestic Violence and the Williams Institute, about 44% of lesbians and 61% of bisexual women have experienced physical violence from an intimate partner. So have 26% of gay men and 37% of bisexual men. That compares to 35% of straight women and 29% of straight men. In the transgender community, studies show somewhere between 31% and 50% have been victims of domestic violence. The National Institutes of Health (NIH) reports there are more cases of domestic violence among men living with male partners than among men living with female partners. (https://newsisout.com/2024/10/breaking-the-silence-lgbtq-domestic-violence-too-often-overlooked/28065/)
- Transgender folks also experience some of the highest levels of intimate partner violence with 54% of individuals reporting an instance of IPV. Nearly one-quarter (24%) have experienced “severe physical violence by an intimate partner.” - https://www.phila.gov/2022-10-05-intimate-partner-violence-in-lgbtq-communities/
Most studies found a lifetime prevalence of intimate partner violence among LGBT people that is as high or higher than the general population.
among 1,608 transgender women, 59.7% experienced certain forms of violence and harassment and 17.7% reported suicidal ideation during the past 12 months; 75.2% reported high social support from significant others, 69.4% from friends, and 46.8% from family. (https://www.cdc.gov/mmwr/volumes/73/su/su7301a7.htm)
- The CDC found that 43.8% of lesbian women reported experiencing physical violence, stalking, or rape by their partners, with two thirds (67.4%) reported exclusively female perpetrators.
- Also, 61.1% of bisexual women reported physical violence, stalking, or rape by their partners in the same study with 89.5% reporting at least one perpetrator being male.
- In contrast, 35% of heterosexual women reported having been victim of intimate partner violence, with 98.7% of them reporting male perpetrators exclusively. (https://www.cdc.gov/violenceprevention/pdf/nisvs_sofindings.pdf)
- 43.8% of lesbian women and 61.1% of bisexual women have experienced rape, physical violence, and/or stalking by an intimate partner at some point in their lifetime, as opposed to 35% of heterosexual women.
- 26% of gay men and 37.3% of bisexual men have experienced rape, physical violence, and/or stalking by an intimate partner in their lifetime, in comparison to 29% of heterosexual men.
- In a study of male same sex relationships, only 26% of men called the police for assistance after experiencing near-lethal violence.
- In 2012, fewer than 5% of LGBTQ survivors of intimate partner violence sought orders of protection.
- Transgender victims are more likely to experience intimate partner violence in public, compared to those who do not identify as transgender.
- Bisexual victims are more likely to experience sexual violence, compared to people who do not identify as bisexual.
- LGBTQ Black/African American victims are more likely to experience physical intimate partner violence, compared to those who do not identify as Black/African American.
- LGBTQ white victims are more likely to experience sexual violence, compared to those who do not identify as white.
- LGBTQ victims on public assistance are more likely to experience intimate partner violence compared to those who are not on public assistance. - https://ncadv.org/blog/posts/domestic-violence-and-the-lgbtq-community
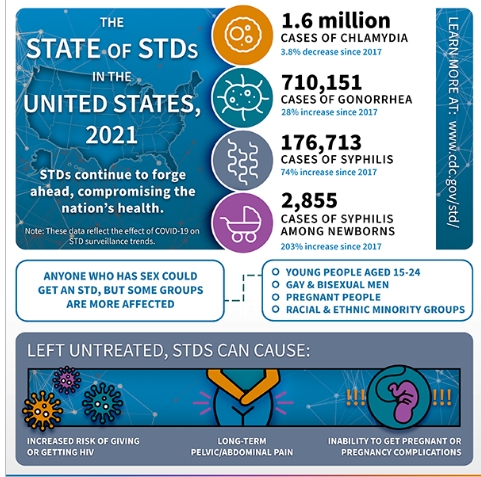
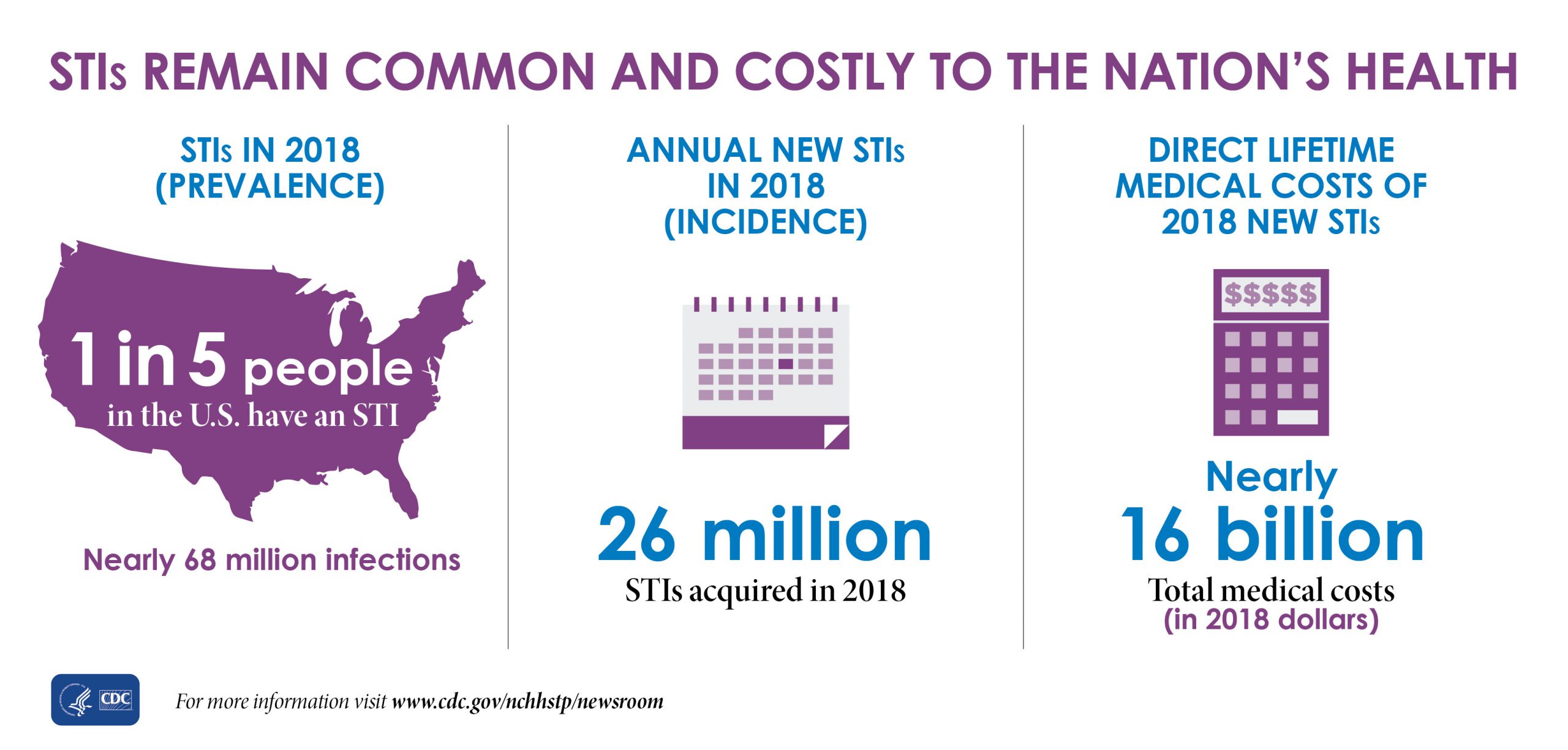
In addition are CDC stats that also include many STDs, which mainly are a result of heterosexual fornication.
In 2021 the CDC estimated that 1 in 5 people in the U.S. have a sexually transmitted infection and at a cost to the U.S. healthcare system of billions of dollars annually. (https://www.cdc.gov/media/releases/2021/p0125-sexualy-transmitted-infection.html)
(Note that in dealing with comparative statics as is done here, not only is the rate or percentage more revealing than simply the number of cases, but also relevant aspects of the historical context.
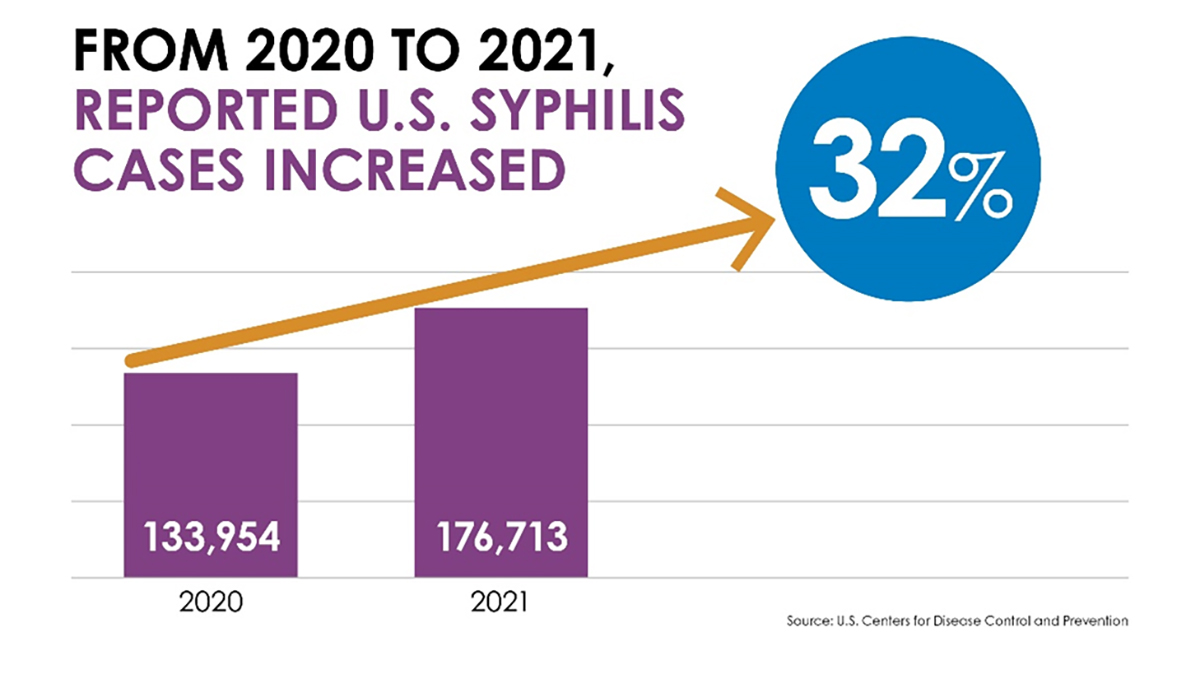
For instance, while the rate of cases of syphilis was actually higher in the 1940's (especially) and overall (with exceptions) decreasing until 2006 when it began an overall steady increase, the historical context of the former included aspects such as increased testing and diagnosis, soldiers returning from war, but with increased effective treatment with penicillin in the 1940s onward leading to a large decrease in transmission, and overall steady decrease in infection rates despite the increased % of teens to middle ages from the 60's to mid 80s. Which, after a brief increase in 1987 to 1992, saw an overall steady and significant decrease until about 2012 (but nowhere close to the 1940's). After which an overall steady rise occurred, leading to a rate of 53.2, which has not been seen since 1919 and 1966.
In contrast, gonorrhea saw unprecedented high rates from 1970 to 1990 when they began to overall steadily fall to a rate of 98.1 in 2009, only to rise to 214, not seen since 1991. (https://www.cdc.gov/std/statistics/2021/tables/1.htm) All of which is despite an increasingly aged population and better testing and treatment.)
Half of all sexually active people will get an STD by the time they reach 25. (https://medalerthelp.org/blog/std-statistics/)
Also relevant, by 2021 the percentage of 18-24-year-olds who were married was 5% for men and 8% for women. with more cohabitating (fornicating) than were married (https://www.bgsu.edu/ncfmr/resources/data/family-profiles/brown-manning-relationship-status-trends-age-gender-fp-21-25.html)
About half (54%) of adolescents age 15-19 have had some type of sexual experience. (https://www.sciencedirect.com/science/article/pii/S2590151621000113?via%3Dihub)
Never-married adults report engaging in sexual relations approx. 14 times per year more than married adults. (https://www.researchgate.net/publication/314273096_Declines_in_Sexual_Frequency_among_American_Adults_1989-2014)
Single Americans over 45 engage in sexual relations more than married ones. (https://www.aarp.org/relationships/love-sex/info-05-2010/2009-aarp-sex-survey.html
By 2008 a CDC study estimated that one in four (26 percent) young women between the ages of 14 and 19 in the United States -- or 3.2 million teenage girls -- was infected with at least one of the most common sexually transmitted diseases (human papillomavirus (HPV), chlamydia, herpes simplex virus, and trichomoniasis). (https://www.sciencedaily.com/releases/2008/03/080312084645.htm) And note that only 33%of women even between age 20-34 are married.
In 2017 it was estimated that about 45 percent of U.S. men and women were infected with the cancer-causing human papillomavirus (HPV sexually transmitted disease - the most common sexually transmitted disease among men and women in the United States. Among women, the prevalence of HPV infection drops to about 22 percent as they age, but it remains high among men. (https://www.webmd.com/sexual-conditions/hpv-genital-warts/news/20170119/nearly-half-of-us-men-infected-with-hpv-study-finds)
The 1995-1999 CDC STD Surveillance Reports state: “During the past two decades, the age of initiation of sexual activity has steadily decreased and age at first marriage has increased, resulting in increases in premarital sexual experience. …”Non-marital sexual activity with multiple partners is the singular cause of the proliferation of STDs and yet for some reason all CDC surveillance reports since 1999 omit the above statement and make no reference to marriage at all. Instead we get, “talk openly about STDs” and the obligatory, “use condoms.” (https://chicago.suntimes.com/2016/12/6/18344396/opinion-as-marriage-rates-decline-reports-of-stds-rise)
Since 2000, rates of P&S syphilis have increased among men, primarily attributable to increases in cases among MSM. Similar to past years, in 2018, MSM accounted for the majority (53.5%) of all reported cases of P&S syphilis and, of these, 41.6% were known to be living with diagnosed HIV. Although rates of P&S syphilis are lower among women, rates have increased substantially in recent years, increasing 30.4% during 2017–2018 and 172.7% during 2014–2018, suggesting a rapidly growing heterosexual epidemic.
In 2000 and 2001, the national rate of reported primary and secondary (P&S) syphilis cases was 2.1 cases per 100,000 population, the lowest rate since reporting began in 1941 (Figure 35, Table 1).
However, the P&S syphilis rate has increased almost every year since 2001. This rise in the rate of reported P&S syphilis has been primarily attributable to increased cases among men and, specifically, among gay, bisexual, and other men who have sex with men (MSM). MSM account for the majority of P&S syphilis cases and estimated rates are substantially higher among MSM compared with women or men who have sex with women only (MSW). 5 The number of cases among MSM has continued to increase, but within the last five years, cases among MSW and women have increased substantially as well. The increase in syphilis among women is of particular concern because it is associated with a striking and concurrent increase in congenital syphilis.
Centers for Disease Control and Prevention: STD Surveillance 2018 National Profile 27 West, and 7.2% in the Northeast (Table 29). Among women, the largest increases were observed in the West (41.2%), followed by the Northeast (40.0%), the South (30.8%) and the Midwest (30.8%) (Table 28). MSM continued to account for the majority of P&S syphilis cases in 2018 (Figures 39 and 41).
Of 35,063 reported P&S syphilis cases in 2018, 18,760 (53.5%) were among MSM, including 16,905 (48.2%) cases among men who had sex with men only and 1,855 (5.3%) cases among men who had sex with both men and women (Figure 39)....
Among the 24,176 male cases with information on sex of sex partners, 77.6% occurred among MSM. A total of 36 states were able to classify at least 70.0% of reported P&S syphilis cases as MSM, MSW, Centers for Disease Control and Prevention: STD Surveillance 2018 National Profile 27 West, and 7.2% in the Northeast (Table 29).
Among women, the largest increases were observed in the West (41.2%), followed by the Northeast (40.0%), the South (30.8%) and the Midwest (30.8%) (Table 28). MSM continued to account for the majority of P&S syphilis cases in 2018 (Figures 39 and 41). Of 35,063 reported P&S syphilis cases in 2018, 18,760 (53.5%) were among MSM, including 16,905 (48.2%) cases among men who had sex with men only and 1,855 (5.3%) cases among men who had sex with both men and women (Figure 39).
Overall, 5,416 (15.4%) cases were among MSW, 4,995 (14.2%) were among women, 5,858 (16.7%) were among men without information about sex of sex partners, and 34 (0.1%) were cases reported with unknown sex. Among the 24,176 male cases with information on sex of sex partners, 77.6% occurred among MSM. A total of 36 states were able to classify at least 70.0% of reported P&S syphilis cases as MSM, MSW, or women each year during 2014– 2018 (Figure 41). In these states, during 2017–2018, the number of cases increased 5.3% among MSM, 16.3% among MSW, and 32.9% among women.
Among 2018 P&S syphilis cases with known HIV status, 41.6% of cases among MSM were HIV-positive, compared with 7.9% of cases among MSW, and 4.0% of cases among women.
When examining reported P+S syphilis cases over time, 36 states were able to classify at least 70% of reported P+S syphilis cases as MSM, MSW, or women each year during 2014–2018. In these states, cases among MSM increased 5.3% during 2017–2018 and 51.5% during 2014– 2018 (Figure 41).
Among males, 610,447 cases of chlamydia were reported in 2018 for a rate of 380.6 cases per 100,000 males (Table 5). The rate of reported cases among males increased each year during 2000–2018, with the exception of 2012–2013, when rates remained stable (Figure 1). During 2017–2018 alone, the rate among males increased 5.7%; during 2014–2018, rates of reported cases among males increased 37.8% (Tables 4 and 5). This pronounced increase among males could be attributed to either increased transmission or improved case identification (e.g., through intensified extra-genital screening efforts) among gay, bisexual, and other men who have sex with men (MSM).
Despite this considerable increase in males, the rate of reported chlamydia cases among females was still about two times the rate among males in 2018, likely reflecting a larger number of females screened for this infection.
Among six jurisdictions participating in SSuN [STD Surveillance Network] continuously from 2010 to 2018,..The estimated gonorrhea case rate among MSM increased 375.5% during 2010–2018 from 1,368.6 cases per 100,000 MSM in 2010 to 6,508.0 cases per 100,000 MSM in 2018. Over the same time period, case rates among MSW and women also increased by 69.3% and 95.2%, respectively.
[Overall,] Rates of chlamydia have gone up by 19 percent since 2014. For gonorrhea, there are 583,405 cases in the U.S., and rates have gone up 63 percent since 2014. Rates of syphilis have increased 71 percent since 2014, and are highest in men and women 25-29 years old. congenital syphilis — when an infected mother passes syphilis to her baby during pregnancy — which have shot up by 185 percent since 2014, (https://www.cdc.gov/std/stats18/STDSurveillance2018-full-report.pdf)
The CDC study Sexually Transmitted Disease Surveillance 2014 found that among male cases for whom the sex of the partner was known, 83% of syphilis cases were MSM. 75.53% of syphilis cases in 2014 were among homosexual men. 51% of the homosexual men diagnosed with syphilis in 2014 were also HIV-positive. (https://www.cnsnews.com/news/article/michael-w-chapman/cdc-83-syphilis-cases-2014-among-gay-men-where-sex-sex-partner-was)
Among women, studies have shown that viral STD rates among bisexual-identifying women aged 15 to 44 years were almost three times higher than women who have sex with women exclusively. (https://www.stdcheck.com/blog/lgbt-std-statistics)
"We estimated an average lifetime HIV-related medical cost for a person with HIV of $420,285 (2019 US$) discounted (3%) and $1,079,999 undiscounted for a median 3-year diagnosis delay and 3% base dropout rate. Our discounted cost estimate was $490,045 in our most favorable scenario and $326,411 in our least favorable scenario."
The cost for PrEP medication was about 2,000 a month, and which "Most health insurance plans, including Medicaid, cover." (https://www.plannedparenthood.org/learn/stds-hiv-safer-sex/hiv-aids/prep) Under the Affordable Care Act, PrEP must be free under almost all health insurance plans. (https://www.cdc.gov/hiv/basics/prep/paying-for-prep/index.html) The rule says insurers must not charge copays, coinsurance or deductible payments for the quarterly clinic visits and lab tests required to maintain a PrEP prescription. (https://www.nbcnews.com/nbc-out/out-health-and-wellness/prep-hiv-prevention-pill-must-now-totally-free-almost-insurance-plans-rcna1470)
In 2017, around 61,300 people were actively taking PrEP.
A few states have their own drug assistance programs that cover out-of-pocket expenses for PrEP. Some will also cover the costs of doctor visits and lab tests. Requirements to qualify for these programs differ by state. (https://www.talktomira.com/post/how-much-is-prep-how-to-get-it-for-free-truvana-descovy)
EDIT: "the federal government has announced that almost all health insurers must cover the HIV prevention pill, known as PrEP, or pre-exposure prophylaxis, with no cost sharing — including for the drug itself and, crucially, for clinic visits and lab tests...This means...Truvada or Descovy, the two approved forms of PrEP, should now be totally free for almost all insured individuals....when taken daily, the tablet reduces men’s risk of contracting the virus from sex with other men by more than 99 percent...PrEP use remains largely limited to white gay and bisexual men... (https://www.nbcnews.com/nbc-out/out-health-and-wellness/prep-hiv-prevention-pill-must-now-totally-free-almost-insurance-plans-rcna1470)
A one-month supply of Truvada or Descovy costs around $2,000. Add in $15,000 a year for the lab tests and doctor visits you'll need to get your prescription. Generic versions of PrEP pills are available and less expensive. They cost about $60 a month. The Affordable Care Act requires most private insurance plans to cover the full cost of PrEP medications, plus lab tests and clinic visits, although not all of them do. PrEP is also covered under Medicare, Medicaid, and the Veterans Administration (VA).Apretude is $3,700 per shot, or more than $22,000 a year. There is no generic form of the injection.(https://www.webmd.com/hiv-aids/prep-choose-medication)
All of the above raises raises private insurance rates and or taxes for all who pay them.
Based on 2022 inflation-adjusted dollars, the US government spent $314 million potentially related to TDF-FTC for PrEP development, including $143 million directly linked to development and clinical testing. (https://www.ajmc.com/view/us-government-spent-far-more-on-costly-hiv-prep-development-than-previously-thought)
Such are just part of the financial and societal costs that affect every one to varying degrees due to man disobeying God's program, in which sexual union is only between male and female in marriage. And which provides the stable safe environment for trust and intimacy and for children which are to result, versus fornication as well as artificial contraceptives.
However, not only is the practice of sexual sin promoted, but war is waged against all who do not agree with such, which includes the tactical, indiscriminate psychological use of the term “homophobic” as part of the overall strategy to misrepresent any all who object to homosexuality and its homoeroticism as being motivated by an irrational fear, and as hate-mongering KKK types.
The idea that one can be caring, charitable, and friendly toward practicing homosexuals while peaceably opposing homosexuality and its relations, is not to be allowed by those who demand we affirm this.
In addition,
since the practice of homosexual relations is unnatural, it
usually requires greater attempts at rationalizing away the guilt
that sin normally should result in, and many even engage in
strenuous attempts to insist all must affirm it.
Which effects mean rejection of the Lord Jesus, leaving the sinner with no forgiveness and more repressed guilt, or worse, a seared conscience that will not repent and which finally may no longer be able to. Which state is to be avoided at all costs.



)